Slowing down Parkinson’s disease isn’t just about medication.
It’s about understanding that the body is far more than a sum of its parts—it’s an intelligent, interconnected system. This condition doesn’t begin in isolation, and it certainly doesn’t progress in isolation either. Parkinson’s is not just a neurological or cognitive issue; it’s a reflection of deeper imbalances across the body, mind, and lifestyle.
I remember a client, Mr. Vinod Mangaldas. What a rockstar!
Seventy-one years young and living with Parkinson’s for the last four years. When I met him during a visit to Coimbatore, he walked up to me, smiled, and said, “I’ve arrested my condition… at 71.” And I knew exactly what he meant.
Yes, he’s on medication to manage tremors, but what truly stood out was everything he was doing beyond that. A clean diet, regular gym workouts, climbing stairs to his office, oil massages, listening to music, staying disciplined; he had adopted an integrative lifestyle.
We’ve now supported him with a protocol to reduce inflammation and enhance brain health. His story is living proof that slowing down Parkinson’s disease is possible when we address the whole person, not just the symptoms.
Let’s be clear—this isn’t a conversation about cures. It’s about perspective. It’s about using real tools to empower ourselves. Food, rest, stress, emotional regulation, and daily habits can play a significant role in slowing down Parkinson’s disease.
Because Parkinson’s rarely arrives unannounced. The body often whispers before it screams. Digestive issues, disturbed sleep, emotional flatness, or a fading sense of smell—these can be early warning signs of Parkinson’s.
Table of Contents
ToggleThe Mind-Body Connection: How Emotions Shape the Nervous System
In the rush to talk about tremors, dopamine, and degeneration, we often miss one of the most critical and healing conversations in Parkinson’s: the emotional terrain in which the nervous system operates.
Today, neuroscience is beginning to echo what ancient healing systems have always emphasized: emotions shape biology. They leave imprints not just in our memories, but within the very wiring of our nervous system. And over time, these emotional imprints can influence everything from neurotransmitter activity to inflammation and cellular resilience.
We’ve long understood Parkinson’s disease as a condition of dopamine loss.
While that’s true biochemically, it paints only part of the picture. Parkinson’s is a nervous system disorder, one that’s intricately linked with chronic emotional stress, suppressed feelings, and unprocessed trauma. This isn’t just theory—it’s physiology.
1. Chronic Stress and Dopamine Depletion
Chronic stress doesn’t just affect mood—it directly impacts the dopaminergic system. When the HPA axis (hypothalamic-pituitary-adrenal) is constantly activated, cortisol levels rise. Persistent cortisol elevation, in turn, has been shown to suppress dopamine synthesis and accelerate neuronal degeneration. According to a study in Biobehavioural Processes, prolonged stress not only worsens Parkinsonian symptoms but also impairs motor control by compromising dopamine signaling.
So, when we talk about managing or slowing down Parkinson’s disease, we can’t ignore the emotional roots of stress physiology.
2. The Autonomic Nervous System and Emotional Memory
The autonomic nervous system (ANS) carries more than just physiological signals—it also holds the residue of unprocessed emotions. Unlike memories stored in the brain, these experiences live as states in the body: tight shoulders from unspoken anger, shallow breath from chronic fear, digestive dysfunction from grief. When the body remains in ‘fight-or-flight’ mode, it suppresses the body’s natural repair systems—fueling fatigue, tremors, sleep disruption, and inflammation.
In Parkinson’s, where the nervous system is already vulnerable, this ongoing sympathetic dominance can worsen the very symptoms we aim to ease.
3. Emotional Dysregulation as an Early Warning Sign for Parkinson’s
Long before the classic motor signs appear, the nervous system may express its imbalance through non-motor symptoms—chronic constipation, sleep disturbances, anxiety, and emotional flatness. These are often misdiagnosed or dismissed, yet they may be among the early warning signs of Parkinson’s. They’re not just psychological, they’re neurological cries for balance.
The terrain for neurodegeneration is often laid quietly, in the body’s attempt to hold emotions that never had a safe place to land.
4. Trauma and Neurological Vulnerability
A 2021 study in Movement Disorders revealed a striking correlation: individuals with PTSD had a significantly increased risk of developing Parkinson’s. Trauma, especially in early life, disrupts neurological regulation, increases inflammation, and impairs dopaminergic pathways.
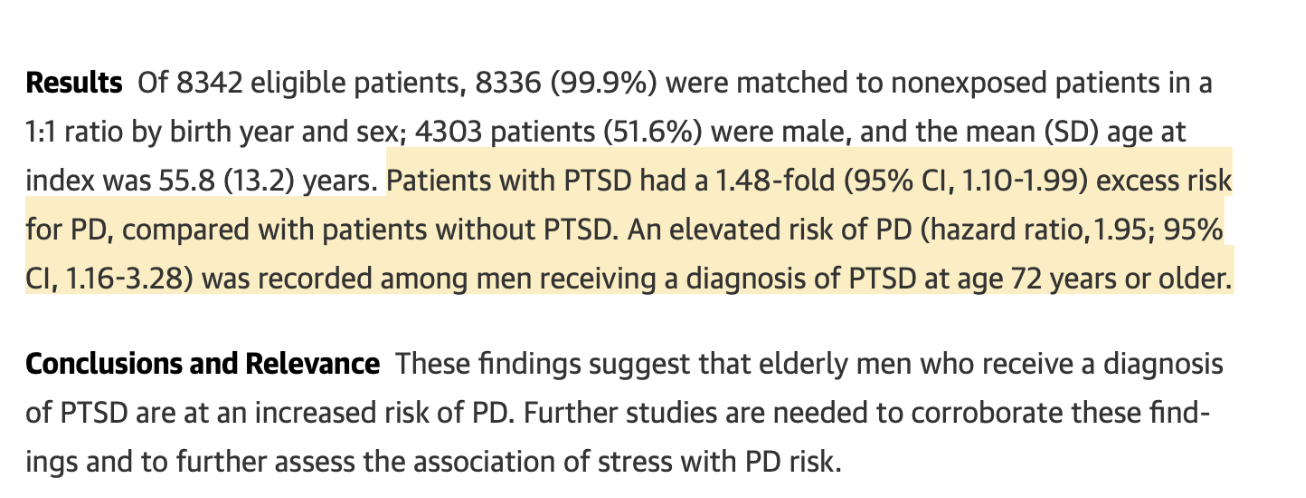
In short, unresolved trauma can tilt the nervous system out of balance, setting the stage for neurodegeneration. This doesn’t mean trauma causes Parkinson’s—but it does mean it’s part of the internal environment that can accelerate it.
Environmental Toxins and Parkinson’s: The Hidden Culprits
When we think about slowing down Parkinson’s disease, nutrition, stress, and exercise usually take center stage. But there’s another silent player in the background—one that often goes unnoticed yet can powerfully influence the brain’s health: environmental toxins.
Emerging research continues to connect exposure to certain chemicals with an increased risk of neurodegenerative conditions, particularly Parkinson’s. While genetics may load the gun, it’s often environmental factors that pull the trigger.
One of the strongest links? Pesticides and herbicides. Numerous studies, including a well-documented review in Neurology (2016), have shown that people with long-term exposure to agricultural chemicals—especially those living in rural areas—have a significantly higher risk of developing Parkinson’s. These chemicals can cross the blood-brain barrier and directly interfere with mitochondrial function and dopamine production, two cornerstones of Parkinson’s pathology.
Then come heavy metals like lead and mercury. These metals are neurotoxic—they disrupt dopamine signaling, increase oxidative stress, and interfere with neuronal survival. Prolonged exposure, even in small doses, may lay the foundation for neurological imbalances that manifest years later.
Air pollution is another invisible factor. Fine particulate matter (PM2.5) can travel through the nasal passage and directly impact the brain via the olfactory nerve. Long-term exposure to polluted air has been associated with higher rates of neuroinflammation and cognitive decline—both of which can exacerbate the progression of Parkinson’s.
So what can we do to protect our nervous system?
- Choose organic produce whenever possible to reduce pesticide exposure. Know where your food comes from. The quality of what we eat matters. Pesticides and herbicides, especially those found in grown fruits and vegetables, have been strongly linked to increased risk of Parkinson’s. But we know it’s not always easy to identify what’s truly clean and trustworthy in today’s market.
That’s why we have launched The Pink Tiger initiative, which is always on guard for you. So you don’t have to second-guess every label or ingredient list. When you see the Pink Tiger Stamp, know that it stands for the highest standard of purity, transparency, and trust. Know more here. - Filter your drinking water to reduce heavy metal content.
- Switch to natural, non-toxic cleaning products and personal care items.
- Be mindful of indoor air quality—plants like peace lilies and spider plants help purify air, or consider using HEPA filters.
When it comes to brain health, every small choice counts. While we can’t control every toxin in the world, we can create a safer internal and external environment—one choice, one shift at a time. And that, too, is a powerful strategy in slowing down Parkinson’s disease.
One of the most promising scientific approaches in recent years is the practice of autophagy and fasting.
Autophagy is your body’s natural process of cellular cleanup, helping to break down and remove misfolded proteins like alpha-synuclein, which is heavily implicated in Parkinson’s. Research shows that structured fasting, when done mindfully and safely can activate autophagy, reduce inflammation, and support better neurological function.
The Gut-Brain Axis and Neuroinflammation
Did you know that more than 70% of your immune system resides in your gut? And that the gut produces nearly 95% of the body’s serotonin and plays a role in regulating dopamine?
Gut dysbiosis, an imbalance in the microbiota, can contribute directly to increased intestinal permeability (leaky gut), allowing endotoxins like lipopolysaccharides (LPS) to enter circulation. These toxins activate systemic inflammation, which in turn fuels neuroinflammation and accelerates the neurodegenerative cascade seen in Parkinson’s.
What’s more, gut-related symptoms like constipation and bloating are now recognized as some of the earliest warning signs of Parkinson’s, appearing years—sometimes decades—before motor symptoms. This further reinforces the importance of food and microbiome diversity in the prevention and progression of the disease.
By focusing on anti-inflammatory, whole-food nutrition, we not only support brain health—we rebuild gut resilience, reduce the inflammatory load, and give the nervous system the environment it needs to function with more ease.
So the next time you sit down for a meal, remember this: it’s not just about what’s on your plate. It’s about what message you’re sending your cells.
Every bite we take is information for our brain—either calming the fire or stoking it.
And in the journey of slowing down Parkinson’s disease, food isn’t a side conversation. It’s one of our most powerful interventions. Not in theory—but in action, at the cellular and systemic level.
The Building Blocks: How Food Influences Dopamine
Let’s talk about dopamine—not just as a neurotransmitter, but as a reflection of the body’s deeper terrain. Because when we talk about slowing down Parkinson’s disease, we can’t ignore the role that nutrition and lifestyle play in supporting the very molecule we often associate with movement, motivation, and mood.
Dopamine is more than a chemical—it’s communication. It’s the language your brain uses to tell your body how to move, feel, and function. And in Parkinson’s, where the gradual loss of dopamine-producing neurons becomes the hallmark, it’s easy to feel like this process is out of our hands. But here’s the truth: while we can’t control every neuron, we can absolutely influence the environment in which those neurons live.
This is where food becomes more than fuel—it becomes functional medicine.
Dopamine is synthesized from an amino acid called tyrosine, which comes from protein-rich foods. Once tyrosine enters the brain, it’s converted into dopamine through a cascade of enzymatic reactions, supported by specific vitamins and minerals. So yes, the food you eat can directly influence your brain’s capacity to produce dopamine—and this matters, especially in the early stages of Parkinson’s or when addressing early warning signs of Parkinson’s like fatigue, mood changes, constipation, or reduced motivation.
Let’s look at a few key nutrients involved in this pathway:
1. Tyrosine: Foods like almonds, pumpkin seeds, bananas, avocados, and legumes are rich in tyrosine. Increasing dietary tyrosine can improve cognitive performance and dopamine-related function, particularly in individuals under stress.
2. Vitamin B6, B12, and Folate: These B-vitamins are essential cofactors in dopamine synthesis and also support methylation, a biochemical process critical for cleansing and brain health.
3. Magnesium: Magnesium supports nerve function, stress modulation, and muscle relaxation. Magnesium deficiency is common in neurodegenerative conditions and may contribute to rigidity and tremors.
4. Coenzyme Q10 (CoQ10): Mitochondria, your cellular energy factory, are particularly vulnerable in Parkinson’s. CoQ10, a compound found in the inner mitochondrial membrane, supports energy production and acts as an antioxidant.
5. Omega-3 Fatty Acids: Found in flaxseeds, chia seeds, walnuts, and fatty fish, omega-3s play a role in modulating inflammation and supporting membrane fluidity in brain cells.
6. N-Acetylcysteine (NAC): NAC helps boost glutathione, the body’s master antioxidant. In Parkinson’s, glutathione levels in the substantia nigra (the brain area that produces dopamine) are often depleted.
7. Vitamin D: Vitamin D isn’t just about bones. It modulates immunity, reduces inflammation, and supports neuroplasticity. That’s why sunlight exposure can help support healthy levels.
Foods for Parkinson’s Disease
We often think of food as fuel or nutrition, but let’s take that conversation deeper, especially when it comes to slowing down Parkinson’s disease. Because food isn’t just about calories or vitamins. It’s information. It’s messaging. Every single bite sends a biochemical signal to your cells, your immune system, your gut, and yes, your brain.
And for someone with Parkinson’s, this becomes even more relevant.
Why?
Because behind the tremors, stiffness, and motor symptoms lies a common, often silent driver: neuroinflammation.
Now, here’s where food enters the picture. Certain foods, especially those high in refined sugars, trans fats, and inflammatory oils, don’t just burden your metabolism—they actually amplify neuroinflammation. Food high in ultra-processed ingredients can fuel systemic inflammation that crosses the blood-brain barrier and contributes to the very pathology we’re trying to manage.

We now have substantial evidence supporting specific anti-inflammatory foods for Parkinson’s disease, which don’t just nourish the brain but modulate the immune system, support gut integrity, and reduce oxidative stress. Let’s explore a few of them:
- Turmeric (curcumin): A potent anti-inflammatory compound that reduces neuroinflammation and protects dopaminergic neurons.
- Omega-3 rich seeds (chia, flax, hemp): These provide essential fatty acids that modulate inflammation and promote neuronal membrane integrity.
- Green leafy vegetables and cruciferous greens: Rich in antioxidants, folate, and phytochemicals that reduce oxidative stress and support methylation—a key pathway in neurotransmitter synthesis.
- Berries: High in anthocyanins and flavonoids, which cross the blood-brain barrier and scavenge free radicals implicated in neurodegeneration.
- Garlic and onions: These support immune modulation, gut microbiome diversity, and have been shown to reduce inflammatory markers in both the gut and the brain.
- Extra virgin olive oil: It is rich in polyphenols like oleocanthal, which have been shown to inhibit neuroinflammatory signaling.
Disclaimer: The food suggestions are intended for general awareness and educational purposes only. Every individual is unique, and what works for one person may not suit another, especially when managing a condition like Parkinson’s. Please do not self-prescribe or make significant changes to your diet without consulting your healthcare practitioner.
What to Avoid in Foods for Parkinson’s Disease
Not all foods nourish. Some deplete, inflame, or disrupt neurological balance. You must avoid:
- Processed Sugar
Spikes inflammation and accelerates oxidative stress. Swap with raw honey or jaggery occasionally, but limit refined sugar entirely. - Excessive Caffeine
Can heighten anxiety and interfere with sleep—two things the brain doesn’t need more of. - Refined Vegetable Oils
Often rich in omega-6s, these oils promote neuroinflammation and damage cellular membranes. Avoid oils like soybean, sunflower, and corn oil. Choose cold-pressed alternatives like coconut, mustard, or extra virgin olive oil instead.
Mind-Body Practices for Slowing Parkinson’s Progression
When it comes to slowing down Parkinson’s disease, we can’t only focus on food or medication. Movement, mindfulness, and emotional regulation play just as crucial a role. The brain and body aren’t separate systems—they’re part of the same intelligent design. And when we engage the mind-body connection intentionally, the nervous system has space to recalibrate, regenerate, and build resilience.
1. Yoga: Movement That Heals
- Parkinson’s affects balance, posture, and coordination—yoga gently rebuilds these from the inside out. But beyond movement, yoga also brings stillness to the mind and nervous system.
- Start with simple routines focused on grounding postures, spinal flexibility, and balance. Even 20 minutes, 3–4 times a week, can make a difference over time.
2. Breathwork and Meditation: Rewiring Stress Pathways
- Chronic stress and emotional tension contribute to neuroinflammation and dopaminergic imbalance—two core issues in Parkinson’s progression.
- Breathwork activates the parasympathetic nervous system, helping shift the body from survival into healing. Meditation improves emotional regulation, which can ease some early warning signs of Parkinson’s like anxiety and sleep disruption.
- Begin your day with 5–10 minutes of alternate nostril breathing, followed by 5 minutes of meditation. Over time, this becomes your nervous system’s daily reset button.
3. Sleep: Your Brain’s Repair Mode
- Without deep, quality sleep, the body can’t initiate autophagy—the cellular cleanup process crucial for slowing down Parkinson’s disease.
- During sleep, the brain’s glymphatic system flushes out toxins. Poor sleep disrupts this, increasing neurodegeneration risk.
- Prioritize a consistent bedtime. Eliminate screens an hour before sleep. Consider calming practices like Yoga Nidra or warm herbal teas to ease into rest.
4. Music and Dance: Dopamine Through Joy
- When movement becomes difficult or robotic, music reconnects the body with rhythm and expression. It’s joy in motion—and joy is therapeutic.
- Rhythmic movement to music can stimulate natural dopamine production, improve gait, and reduce motor rigidity.
- Play music you love and move freely, without rules. Even a few minutes daily can reawaken motor pathways and shift emotional states.
5. Journaling: Releasing What the Body Holds
- Emotional suppression is common in chronic illness, and yet, unresolved feelings silently weigh down the nervous system, increasing internal stress.
- Writing helps reduce cortisol, improve immune function, and increase self-awareness.
- Create a 10-minute evening journaling ritual. Let your thoughts out without judgment. The clarity and emotional release that follow are deeply healing.
The Path Ahead: Consistency, Not Perfection
Your emotions are not separate from your symptoms. They’re part of your body’s language and in Parkinson’s, they might be among the earliest whispers before the nervous system begins to shout.
So if you’re on a journey of slowing down Parkinson’s disease, don’t ignore the emotional chapters of your story. Honor them. Sit with them. Work through them. Because emotional healing is neurological healing.
And as always, start small, but start somewhere.
Disclaimer: This blog is meant for informational and educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. The insights shared are not a substitute for professional medical advice or care. If you are living with Parkinson’s disease or any other medical condition, please consult your healthcare provider before making any changes to your lifestyle, medication, or nutritional plan. What’s shared here is not one-size-fits-all.
If you or a loved one is living with Parkinson’s and you’re exploring ways to complement your current care with lifestyle support, with Luke’s Wellness Program, where real transformation begins.
Because true change isn’t about intensity, it’s about consistency done right.
Schedule a one-on-one consultation with our experts by calling us at 1800 102 0253 or emailing us at [email protected].
Team Luke
Start Your Wellness Journey
Feeling inspired to take the next step in your wellness journey? Connect with us to explore how our tailored programs can support your health journey. Your transformation is just a conversation away.



